CRISPR gene editing has revolutionized the landscape of genetic science, offering unprecedented possibilities for treating hereditary diseases. This cutting-edge technology enables precise alterations in DNA, raising hopes for cures, such as gene editing for sickle cell disease. However, with such potential comes a myriad of ethical issues CRISPR presents, sparking debates among scientists, ethicists, and the public regarding its implications. As health equity in gene editing takes center stage, questions about who has access to these therapies loom large, particularly with the high costs associated with treatments. Furthermore, the risks of CRISPR technology call for robust discussions on bioethics and gene therapy, prompting us to weigh the benefits against the potential downsides of tampering with human genetics.
Gene modification technologies, particularly CRISPR, are unlocking new frontiers in medical science, presenting both hope and ethical dilemmas. This innovative approach to gene alteration allows researchers to edit out genetic disorders at their source, potentially transforming the lives of countless individuals suffering from inherited conditions like sickle cell. However, as these advancements unfold, they bring forth complex conversations surrounding the morality of altering human DNA and the socio-economic disparities that may result from selective access to gene therapies. The implications of health equity surrounding genetic editing highlight a burgeoning divide in who benefits from such scientific progress. As we navigate this brave new world of gene editing, the balance between scientific innovation and ethical responsibility remains a pressing concern.
Ethical Implications of CRISPR Gene Editing
The emergence of CRISPR technology has revolutionized the field of gene editing, but it has also raised significant ethical implications that cannot be ignored. Key concerns revolve around the morality of altering human DNA and the potential repercussions of such modifications on society as a whole. During the discussion, speakers highlighted how the ability to edit genes introduces complex questions about the nature of human variation and the societal expectations surrounding health and disease. For instance, should we intervene in the genetic makeup of embryos for ailments that, while challenging, do not severely impair quality of life, such as Down syndrome? This question not only reveals the delicate balance between medical advancements and ethical standards but also challenges our notions of disability and what it means to be human.
Moreover, the conversation on ethics extends to considerations of parental choices in genetic modifications. Should parents have the ultimate authority to decide traits for their offspring, even when those traits reflect personal values or societal biases? The implications of such decisions are profound, touching on issues of autonomy, consent, and the potential stigmatization of those who do not meet societal standards of ‘normalcy.’ Examining these ethical dilemmas is crucial as we navigate the future of CRISPR and its applications in gene editing.
In the realm of bioethics, the risks associated with CRISPR technology also merit serious attention. Beyond the immediate desires to alleviate suffering from genetic disorders like sickle cell anemia, there lies the potential for misuse and unforeseen consequences. For instance, experimenting with germline editing—altering the genetic configuration of embryos—could result in unexpected health issues not just for the edited individual, but for future generations as well. Thus, the question of oversight becomes critical in this unfolding narrative of gene editing technologies. What regulatory frameworks are necessary to ensure responsible practices and prevent unethical applications? The fear of a ‘gene editing race’—where countries may implement CRISPR without oversight—stresses the need for a united global approach to bioethics in gene therapy.
Health Equity and Gene Editing
Equity in healthcare has become a pressing concern in the age of advanced medical technologies such as CRISPR gene editing. The financially prohibitive cost of innovative treatments, exemplified by the sickle cell cure that costs approximately $2.2 million, raises questions about accessibility for marginalized groups. In discussions about health equity, experts emphasize the fundamental right to access health resources, irrespective of socioeconomic status. When advancements in gene editing promise to transform lives, yet remain out of reach for a significant portion of the population, it highlights systemic injustices within healthcare structures. A focus on fairness is essential; as new gene therapies emerge, we must ask who will benefit and who will remain underserved, making health equity a vital issue to address in conjunction with scientific progress.
Furthermore, health equity in gene editing goes beyond economics. It intersects with social determinants of health, including race, geography, and healthcare infrastructure. The conversation led by Neal Baer indicated that the global implications of CRISPR are vast, as many diseases disproportionately afflict communities in low-to-middle-income countries. With the advancements and potential of gene editing, the challenge becomes not only to innovate but also to democratize access to such treatments. The overarching goal should be to foster an environment where every individual, regardless of background, can benefit equally from groundbreaking medical advancements.
The role of education in health equity cannot be overstated, as public understanding of genetic technologies must match the pace of their development. Initiatives that educate both healthcare professionals and the general public can empower individuals to advocate for their health rights, ensuring equitable access to CRISPR therapies. Addressing disparities in education about gene editing, especially in communities that bear the highest disease burden, can help mitigate the risks of exploitation and enhance shared decision-making in health care. Overall, health equity highlights the responsibility of the scientific community to not only consider the cutting-edge breakthroughs of CRISPR gene editing but also to integrate ethical practices that ensure humane application for all layers of society.
The Risks Inherent in CRISPR Technology
Though CRISPR gene editing holds incredible promise for medical breakthroughs, it also carries inherent risks that warrant careful consideration. One major concern is the potential for off-target effects, where unintended modifications occur in genes other than the targeted area, leading to unpredictable outcomes. These consequences can manifest as new health issues or unforeseen genetic disorders that were not part of the original intent of the treatment. This underscores the complexity of genetic interactions and the intricate web of our biological makeup, pointing to the necessity for extensive research and validation before CRISPR can be widely adopted for therapeutic purposes. Therefore, establishing rigorous testing protocols and long-term studies are not just recommended but essential to ensure patient safety and efficacy of gene editing techniques.
Moreover, the ethical implications of using CRISPR extend into the realm of designer genetics, raising fears about humanity’s trajectory. With the capacity to manipulate genes that affect intelligence, athleticism, or aesthetic traits, the boundaries of ethical limits blur. As highlighted in the discussion, creating a generation with potentially engineered ‘superior’ traits opens a Pandora’s box of societal inequities, where only the privileged sectors can afford enhancements. This facet introduces the question of how to govern the application of CRISPR technologies and establish a framework that prevents the emergence of biased socioeconomic divides rooted in genetic capabilities.
In light of these risks, the importance of global dialogue cannot be overstated. As health innovators and researchers around the world push the frontiers of CRISPR technology, international guidelines must be established to govern research and clinical practices. Fostering discussions that include various stakeholders—scientists, ethicists, policymakers, and the public—can lay the groundwork for responsible gene editing that prioritizes safety and ethical standards. In doing so, we can protect against the potential dangers of CRISPR technology while unlocking its full potential for positive impact on health and disease management.
Informed Consent in Genetic Editing
In the evolving narrative of CRISPR gene editing, informed consent emerges as a pivotal component of ethical practice. Patients and parents must fully understand the implications and risks associated with genetic modifications, especially given the complexities and long-term consequences of such decisions. The discussions surrounding bioethics highlighted that informed consent should transcend legal formalities, encompassing genuine understanding and awareness of the potential outcomes. As treatments become more pervasive, ensuring that individuals make empowered decisions about their health requires transparent communication from healthcare providers about the nuances of gene editing technologies and their limitations.
Informed consent also raises issues of autonomy and agency, particularly in the context of germline editing, where the implications of decisions extend beyond the individual to future generations. Parents tasked with making choices for their unborn children must navigate the ethically charged waters of selecting genetic traits or undergoing interventions. Here, the potential for coercion becomes a concern, as societal pressures may influence personal choices. As the conversation in the seminar pointed out, fostering an environment where individuals feel truly free to make informed decisions is essential to uphold ethical standards in genetic editing.
Moreover, the role of ethics boards and oversight committees becomes critically important in the landscape of CRISPR gene editing. Establishing robust protocols for ethical review ensures that proposals for gene editing interventions undergo rigorous scrutiny before implementation. These boards must include diverse perspectives to adequately address the multifaceted ethical challenges that arise with new technologies. Additionally, the inclusion of public opinion in establishing ethical guidelines for gene editing demonstrates a commitment to incorporating societal values in the decision-making process. Therefore, advancing strategies to enhance public literacy on CRISPR and its implications will empower individuals and bolster informed consent practices for emerging genetic therapies.
The Future of CRISPR in Medicine
The future of CRISPR technology presents exhilarating possibilities that could redefine medicine and patient care. As research continues to advance, the potential for CRISPR to address a multitude of genetic disorders expands dramatically. Beyond sickle cell anemia, scientists are exploring applications in treating various inherited diseases, such as cystic fibrosis and muscular dystrophy, aiming for effective solutions that can improve quality of life for countless individuals. This revolutionary capability positions CRISPR as a cornerstone of personalized medicine, where targeted therapies are tailored to the unique genetic profile of each patient, offering hope for chronic conditions previously deemed untreatable.
However, as we look toward the future of CRISPR, careful consideration of its implications is necessary. The rapid pace of technological advancement often outstrips regulatory frameworks, raising the urgency for evolving policies that address emerging ethical concerns. Global collaboration between scientists, lawmakers, and ethicists is vital in creating a holistic approach that can safeguard patient welfare and public trust in gene editing technologies. In forging a path forward, we must strike a balance between exploration of CRISPR’s potential and the assurance of ethical compliance.
Additionally, public engagement plays an essential role in shaping the trajectory of CRISPR technology. Open forums that encourage dialogue between scientists and the community can demystify the science of gene editing, empowering individuals to voice their opinions on the direction of these advancements. Advocacy for transparency in clinical trials and ongoing public education initiatives about the risks and rewards of gene therapy can cultivate a more informed society. Ultimately, the future of CRISPR in medicine hinges not only on scientific breakthroughs but also on our ethical commitments and collective governance frameworks that reflect the values of humanity.
Frequently Asked Questions
What are the ethical issues surrounding CRISPR gene editing?
The ethical issues surrounding CRISPR gene editing mainly include concerns about the morality of altering human traits, the potential for eugenics, and the implications of editing germline genes that affect future generations. It raises questions on whether we should prioritize disease eradication over natural human diversity and how we decide which traits are subject to alteration.
How does CRISPR gene editing help in the treatment of sickle cell disease?
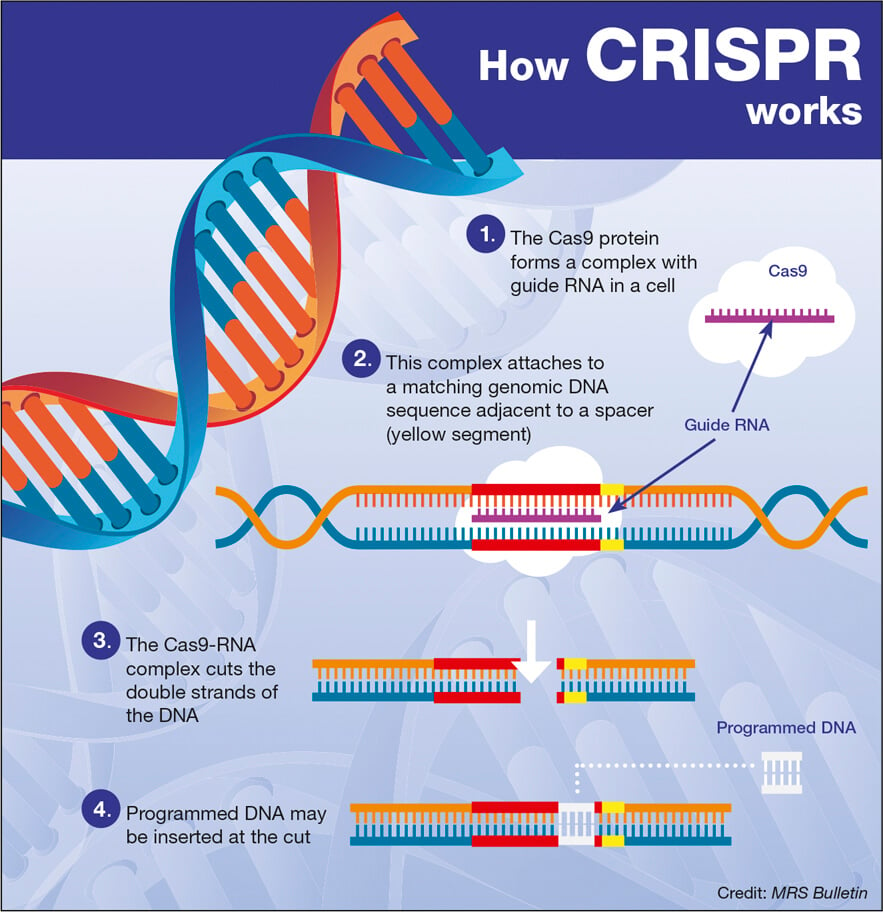
CRISPR gene editing offers a promising treatment for sickle cell disease by targeting and modifying somatic cells to eliminate the genes causing the disease. This technology allows for significant advancements in gene therapy, providing a potential cure for many affected individuals.
What are the risks associated with CRISPR technology?
The risks associated with CRISPR technology include unintended genetic changes, ecological consequences from gene editing in organisms, and potential health issues arising from off-target effects. Concerns also exist regarding the misuse of CRISPR for enhancement purposes rather than just therapeutic applications.
How does health equity play a role in gene editing discussions?
Health equity plays a critical role in discussions about gene editing as the costs and accessibility of treatments like CRISPR-cured therapies may disproportionately benefit wealthier individuals and countries. This raises issues about fairness and the potential widening of health disparities between different populations.
What bioethics considerations are important in the context of gene therapy using CRISPR?
Important bioethics considerations in CRISPR gene therapy include informed consent from patients, especially in germline editing where future generations are affected, equitable access to treatments, and the oversight of research to prevent unethical uses of gene editing technology.
Can CRISPR technology be used for enhancement rather than for curing diseases?
Yes, CRISPR technology can potentially be used for enhancement, leading to ethical debates about its application for non-medical traits such as intelligence or physical appearance. This raises concerns about the societal implications and whether enhancements could lead to new forms of inequality.
| Key Points |
|---|
| CRISPR technology allows editing of somatic and germline genes, raising ethical questions regarding the extent of genetic modifications. |
| Curing conditions like sickle cell anemia with CRISPR presents issues of access and cost, estimated at $2.2 million per patient, which could exacerbate health disparities. |
| The ethics of gene editing extend to whether parents should decide on their child’s genetic traits, creating a debate about parental rights vs. human variation. |
| Lack of global oversight on gene editing practices raises concerns about the misuse of technology in countries with fewer regulations. |
| Unintended consequences of gene editing are a risk, as genetic changes may disrupt complex biological interactions. |
Summary
CRISPR gene editing holds immense promise for curing genetic diseases, yet it also presents significant ethical dilemmas. The potential to edit our genes raises fundamental questions about the essence of humanity and the societal implications of such advancements. As we explore the capabilities of CRISPR technology, we must carefully weigh the benefits against the possible moral consequences and ensure equitable access to these transformative treatments.